Dr Gina Kennedy recently attended the Association of British Neurologists (ABN) conference and led a discussion on the prescribing issues around the new anti-CGRP medications. She reports here:

I arrived at Waverley train station in Edinburgh to the distinctive sounds of bagpipes and battled with the cobbled streets and many steps of the old town with my unsuitable 4 wheeled case. The sun did try to shine before a complete washout for 2 days which destroyed a pair of poorly chosen suede ballet pumps.
The Edinburgh International Conference Centre
The Edinburgh International Conference Centre venue was expansive and daunting, the main vast auditorium being 3 escalators up, and the exhibition area was located 2 escalators down from entrance level.
Topics were very varied
There was an impressive, and at times, overstimulating number of parallel and sequential sessions at this year's ABN conference. Topics ranged from the ordinary practical management of common conditions such as encephalitis, CIDP, myasthenia gravis, epilepsy and MS, to the sublime rare presentations of infective (Lyme as a reversible cause of dementia), genetic (POLG mitochondrial disorder), and radiological (CHANTERS Syndrome) conditions.
The Headache Special Interest Group debate: Clinical Headache dilemmas in 2024: MaBs or Pants, Jabs or Tabs: and what about Tox?

On the second day, a selection of breakfast pastries encouraged conference attendees to turn up for the early morning Specialist Interest Group slot allocated to the British Association for the Study of Headache. Dr Nick Silver, The Walton Centre, Liverpool chaired the session with ease and charm, making everyone feel welcome and comfortable. I, Dr Gina Kennedy, South Tyneside and Sunderland, presented the national survey results on the advanced migraine therapies which include Botox, CGRP MaBs and gepants. This was an unfiltered and raw representation of how practitioners in headache are using these treatments in the real world: when to start, stop, review and consider medication breaks.
There was also feedback on who should prescribe, what order, and desired treatment combinations. Dr Krishna Dani, from Glasgow, brought the Scottish perspective with a bit of dry Scottish humour. He also provided a clear overview of potential cautions of CGRP treatments with comorbidities.
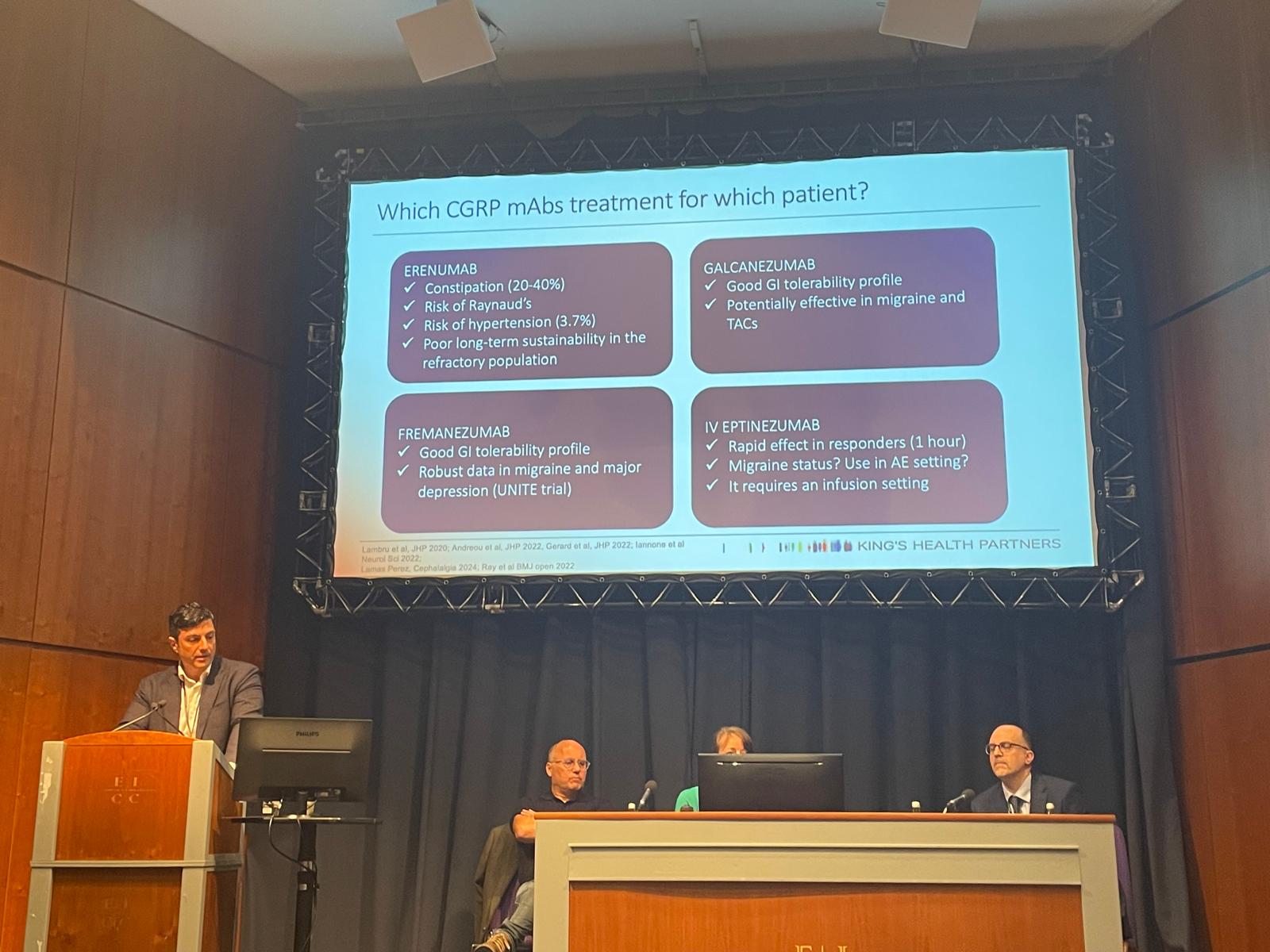
Finally, Dr Giorgio Lambru, from Guy's and St Thomas's, provided a wealth of evidence-based data on CGRP treatment switching and stopping, including data on head-to-head study between a gepant and CGRP MAb.
The audience posed questions on the safety of combination treatments , treatment in pregnancy and accessibility. It was a refreshing opportunity to have frank, honest discussions about the current dilemmas that come with the increasing treatment choices we have in headache.
The overall consensus was that this choice is being shared with the patient more than it has ever been previously, which only serves to empower patients further in their search towards pain freedom.
(Editor's note: You can read the EHF Guidelines for prescribing Monoclonal antibody CGRP drugs from 2022 here. Guidelines for the UK may differ. NICE has issued some guidance on individual medications https://cks.nice.org.uk/topics/migraine/how-up-to-date-is-this-topic/update/ )
Treatment accessibility within Headache services
Other headache updates included four different CGRP symposiums with data on gepants and CGRP monoclonal antibody treatment and discussion about where they fit in practice. A walking tour of the posters on Headache and Pain was interesting also.
There is a current drive by NHS England in optimising efficiencies in Neurology outpatient care based on Getting It Right First Time (GIRFT) strategies within the new Further, Faster approach (Further Faster Programme - Getting It Right First Time - GIRFT).
Advice and guidance was presented as an opportunity to support gepant prescribing within primary care, where that is appropriate, for rescue treatment or certain preventative circumstances where local prescribing formularies allow.
Most regions have a RAG green prescribing status for Rimegepant for acute migraine management, allowing primary care initiation of these treatments. However, there is a wide variation of prescribing restrictions for Rimegepant preventative treatment in episodic migraine from green plus, amber and even red RAG status (The Traffic Light System and Classification of Medicines (Remedy BNSSG ICB)). This means that patient access to gepant preventative medication is turning into a postcode lottery with unacceptable variation around the country. This will need to be addressed via the Integrated Care Boards for each region and reinforces the need to fly the flag for equitable patient access, supported by NHS England programmes such as Further, Faster to improve outpatient service efficiencies.
Clinical case discussions may remind us of rare diagnoses
One of the highlights of the Conference were the clinico-pathological case discussions - an interplay of academic intellect with a forensic detective approach. The most thought-provoking was a migraine-mimic by an underlying deadly fungal aspergillus sphenoid disease. Peri-neural spread to optic nerves, a vascular pseudoaneurysm and basal sub-arachnoid haemorrhage as a complication of aspergillus was only diagnosed post- mortem. I found this a sobering thought when thinking about all the migraine reassurance dispensed over the years. However the case example was an 88 year old lady when our natural alarm bells for secondary causes are ringing loudly, prompting thorough investigation in the real world.
(Editor: a different published case report can be read here and more about Aspergillus here)
A chance to network with colleagues

I enjoyed the opportunity to catch quick greetings with familiar and not-so-familiar faces, wondering if they should be more familiar judging from their enthusiastic welcome. The Gala dinner was well-attended with an eager live band and Ceilidh caller with a successful improvisation on ‘Brown Girl in the Ring’ which fed on the high energy in the room.
Overall, I left a bit soggy but with a fresh perspective on work and life. There was a strengthened sense of being in the same boat with peers across the country which helps one avoid drowning in clinical autonomy.
A thoroughly enjoyable method of CPD and social update, see you all next year!

Dr Gina Kennedy
BASH Scientific Officer
Consultant neurologist, Sunderland
To learn more about prescribing for migraine and other headaches, please see our Guidelines page here